Medication and Pain Management
Pain is familiar to all of us and is probably the most common reason someone sees a doctor. Pain Management is not so familiar, and referral to a pain management specialist can at first be confusing. Pain at times indicates injury, such as a broken bone or a cut, and the reason for the pain is obvious. Pain at other times can be more mysterious, and may represent a symptom of something else, like infection or inflammation. When your pain is thought of as a symptom, like other symptoms such as a fever, cough or rash, diagnosis at times requires referral to a specialist.
Pain Management specialists are specially trained physicians who can evaluate your symptoms and help to make an accurate diagnosis. Having the right diagnosis is the key to having the right treatment. Pain Management specialists are equipped to work with your doctor to help evaluate, diagnose and treat a variety of pain problems. Sometimes evaluation is as simple as an office visit, other times special tests are necessary. Treatment can involve medications, therapy or advanced nerve blocking techniques. The first step to recovery is, of course, the evaluation, so don’t hesitate, take a step!
Common Medical Pain Management Procedures
Today, patients have a wide variety of medications, treatments and procedures to choose from to treat their back pain. Some drugs not only relieve pain but also work to reduce inflammation and relax muscle tension and spasm. However, many of these medications, even those available without a prescription, can have serious side effects. Pain injections of medication onto or near nerves can sometimes significantly help therapeutically to relieve the pain that has not responded well to oral medications. In addition most injection procedure serve doctors diagnostically find or verify the source of pain suspected. The medications that are injected include local anesthetics, steroids, and opioids.
- Blocks with local anesthetic can be used to control acute pain. (Hence, the shot at the dentist or the epidural block for a surgery or a delivery.)
- Pain and injury often makes nerves more sensitive, so that they signal pain with less provocation. Think about lightly brushing against your skin when you have a sunburn. Blocks can provide periods of dramatic pain relief, which promotes the desensitization of sensory pathways.
- Steroids can help reduce nerve and joint inflammation and can reduce the abnormal triggering of signals from injured nerves.
- Blocks often provide diagnostic information, helping to determine the source of the pain.
Remember, blocks are not the best treatment for all pain problems. Patients often ask me, “Doc, can’t you just do a nerve block?” Often blocks are not possible, are too dangerous, or simply are not the best treatment for the problem.
Spinal Injections
The most common spinal injection is the lumbar epidural steroid injection. This is particularly useful for pain that radiates from the lower back into a leg, and is caused by disc herniation or spinal stenosis(narrowing around the nerves) which triggers nerve root irritation. Similar injections can be very useful in the cervical spine, where the symptoms will extend into the arms. Thoracic epidural steroid injections are most commonly used to reduce the pain associated with herpes zoster (shingles). Such blocks may reduce the risk of developing persistent postherpetic neuralgia (i.e., pain which persists long after the skin eruption has healed).
The facet joints of the spine can also cause pain. Injections into the facet joints or blocks of the nerves that go to the facets can often be very helpful with these pains. This problem is more common in the lumbar spine, but also occurs in the neck.
Discograms (intradiscal injections of contrast under fluoroscopy or CT imaging) can determine if and which disc is the source of the pain. This can help a surgeon determine which levels of the spine require surgery. If the patient is found to have a painful disc, they may be a candidate for a new and promising technique, intradiscal electrothermoplasty (IDET). In a procedure similar to a discogram, a wire is temporarily inserted into the disc and used to heat the disc. This destroys the invading sensory nerves and causes the proteins of the disc wall to reshape and slowly strengthen (over 3-6 months). The procedure cannot be done if the disc has already severely degenerated.
Transforaminal Steroid Injections
Epidural glucocorticoid injections are commonly given to patients with leg and/or back pain to relieve such pain and improve mobility without surgery. These steroid injections buy time to allow healing to occur and/or as an attempt to avoid surgery after other conservative (non-surgical) treatment approaches have failed.
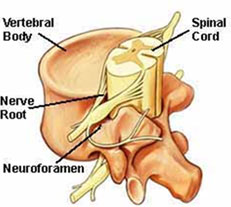
During a transforaminal injection, a small-gauge blunt needle is inserted into the epidural space through the bony opening of the exiting nerve root (See Figure 1, Neuroforamen).
The needle is smaller in size than that used during a conventional epidural approach. The procedure is performed with the patient lying on their belly using fluoroscopic (real-time x-ray) guidance, which helps to prevent damage to the nerve root. A radiopaque dye is injected to enhance the fluoroscopic images and to confirm that the needle is properly placed (See Figure 2). This technique allows the glucocorticoid medicine to be placed closer to the irritated nerve root than using conventional interlaminar epidural approach. The exposure to radiation is minimal.
Spinal Conditions Treated and Outcomes
Indications include large disc herniations, foraminal stenosis, and lateral disc herniations. Patients with disc herniations and leg pain in most of the studies attained maximal improvement in 6 weeks. Interestingly, long-term success rates for transforaminal epidural glucocorticoid injections ranged from 71% to 84%.
Is More than One Injection Necessary?
As a rule, patients who obtained little relief from the first injection got little benefit from a second or third injection. Those patients with degenerative lumbar canal stenosis and patients who failed previous therapies may significantly improve standing and walking tolerance following transforaminal lumbar steroid injections. However, only about 15% to 61% of interventional pain management physicians perform transforaminal epidural injections. Interestingly, almost every single interventional pain management physician uses the conventional, interlaminar epidural injection.
Complications
Complications are rare but may include headaches, infections, blood pressure changes, bleeding, and discomfort at needle insertion site. Use of steroids rarely causes an increase in blood sugar and blood pressure, as well as leg swelling. The major complication, that being damage to a nerve root is very rare. However, using a blunt needle may even more reduce the risk of this complication.
Patient Sedated but Awake
The patient is sedated but awake through the intervention. It is important that the physician and patient communicate during the procedure. If significant leg pain is triggered during placement of the epidural needle or injection of the medication, the physician will immediately stop the procedure and check the position of the needle and the source of pain.
Epidural Steroid Injections
What is an epidural and why is it helpful?
A. An epidural injection places anti-inflammatory medicine into the epidural space to decrease inflammation of the nerve roots, hopefully reducing the pain in the neck, shoulders and arms. The epidural injection may help the injury to heal by reducing inflammation. It may provide permanent relief or provide a period of pain relief for several months while the injury/cause of pain is healing.
What is the epidural space?
A. The membrane that covers the spine and nerve roots in the neck is called the dura membrane. The space surrounding the dura is the epidural space. Nerves travel through the epidural space to the neck, shoulder and arms. Inflammation of these nerve roots may cause pain in these regions due to irritation from a damaged disc or from contract with the bony structure of the spine in some way.
What happens during the procedure?
A. An IV is started so that relaxation medication can be given. The patient is placed sitting in a chair and positioned in such a way that the physician can best visualize the neck using x-ray guidance. The skin on the back of the neck is scrubbed using 2 types of sterile scrub (soap). Next, the physician numbs a small area of skin with numbing medicine. This medicine stings for several seconds. After the numbing medicine has been given time to be effective, the physician directs a small needle, using x-ray guidance into epidural space. A small amount of contrast (dye) is injected to insure the needle is properly positioned in the epidural space. Then, a small mixture of numbing medicine (anesthetic) and anti-inflammatory (cortisone/steroid) is injected.
What happens after the procedure?
A. Patients are then returned to the recovery area where they are monitored for 30-60 minutes. Patients are then asked to record the relief they experience during the next week on a post injection evaluation sheet (pain “diary”). This will be given to the patient when they are discharged home. A follow-up appointment will be made for a repeat block if indicated. These injections are usually done in a series of three (3), about two (2) weeks apart. The arms and hands may feel weak or numb for a few hours. This is to be expected, however it does not always happen.
Vertebral Facet Injections
The therapeutic benefit of facet injections remains controversial. The controversy begins with the poor correlation of the history and examination with true facet mediated low back pain.
Many patients will complain of back and often lower extremity pain with standing, walking, and extension-type activities. The neurologic examination is normal, and provocative tests for nerve root inflammation are usually negative. Many patients will have increased pain on passive extension, and/or extension and rotation; less often patients will complain of pain with flexion. Tramadol is often given as an injection for back pain in hospitals, or your doctor may prescribe the same medication in capsules to take at home. This drug works quickly and effectively. However, it should not be taken too often to avoid addiction.
In addition, radiographic and bone scan imaging has not been helpful in selecting appropriate patients for facet injections. The primary role of facet injections remains diagnostic. There is less support for the therapeutic effect of intra-articular corticosteroid injections or ablations of the nerves innervating the lumbar facet joints.
Facet injections should be used for patients who have failed a directed non-operative treatment program which incorporates various manipulation/mobilization techniques. They are not indicated in the first four to six weeks of treatment and, when utilized, should be done under fluoroscopic guidance using contrast medium to assure proper placement.
The goal of facet injections is to verify the diagnosis and perhaps assist with pain reduction in order to facilitate an active physical therapy program. If prior injections were helpful and there is a recurrence of pain, they can be repeated; however, repeat injections should be limited. Those patients who have reliably demonstrated a therapeutic analgesic response to injected anesthetics of varying half-lives and have failed conservative care may be candidates for therapeutic radiofrequency denervation procedures. This procedure should be used only in those failing a comprehensive program and in no way should be considered in the initial management of an episode of acute low back pain.
Sympathetic Nerve Blocks
What is it?
A. A block that is performed to determine if there is damage to the sympathetic nerve chain and if it is the source of pain. This is a diagnostic test primarily, but it may provide relief far in excess of the duration of the anesthetic. Sympathetic nerves are a network of nerves extending the length of the spine that control some of the involuntary functions of the body such as opening and narrowing blood vessels.
How is it done?
A. A local skin anesthetic is given in the lumbar area of the back. A needle is then inserted into the back under fluoroscopy next to the vertebral body. The block may be performed on both sides of the spine. An anesthetic medication will be injected into the area.
Expected Results
A. The patient may note redness of the lower extremity and a feeling of warmth.
How long does it take?
A. It takes thirty minutes for the procedure followed by evaluation and recovery for several hours.